How to recognize the symptoms of diverticulitis
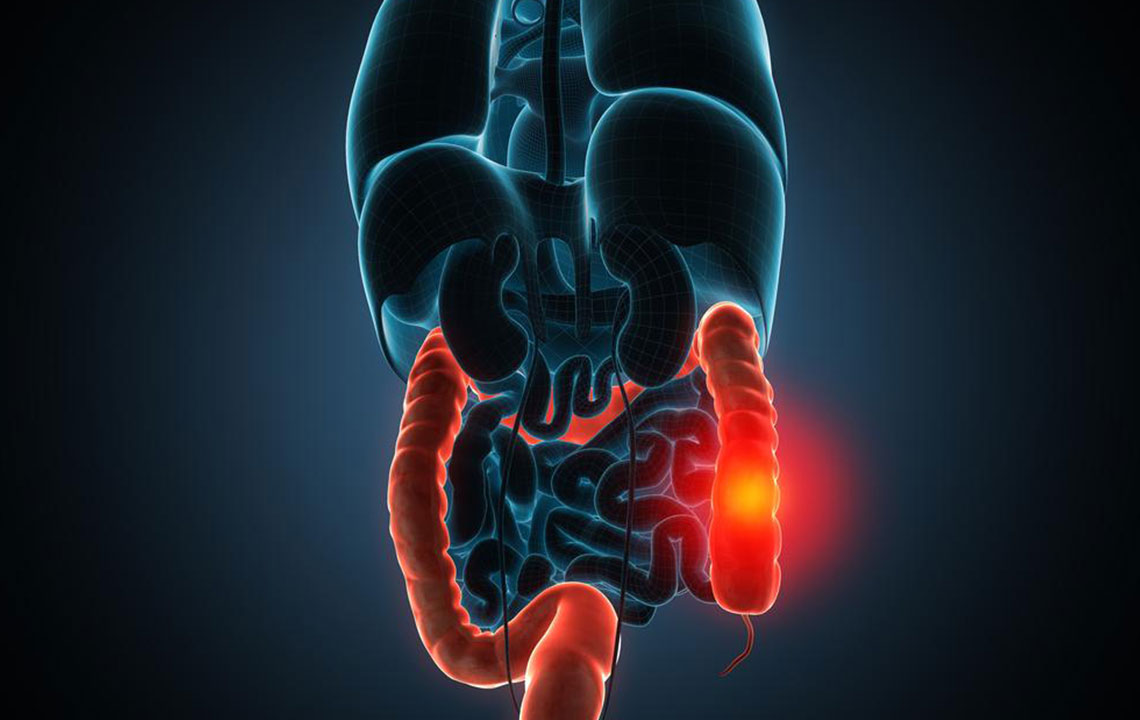
Diverticulitis occurs when the bulging sacs that appear in the lining of your large intestine, or colon, get acutely infected or inflamed. Diverticula are bulging sacs or small blisters that appear in the lining of the large intestine or colon. At the first appearance of the sac, it is called as diverticulosis but when they get acutely inflamed or infected, it is called diverticulitis.
What causes it?
It is very common in the older population. Doctors are still not sure about what exactly causes diverticulosis. But mostly a low-fiber diet is responsible for contributing to the formation of the sacs.
How to identify diverticulitis symptoms
One of the common diverticulitis symptoms is a constant pain in the lower left side of the abdomen. The pain starts below the belly button and moves to the lower left side of the abdomen.
The pain is often worse at the time of food intake, or shortly afterward, if the stool is passed it may help relieve the pain.
Some long-term diverticulitis symptoms include:
- Change in the regular bowel habits marked by constipation or diarrhea, or episodes of constipation that are followed by diarrhea
- Bloating and gas.
- Loss of appetite
- Nausea and vomiting at times
- Fever with high temperature of 38 degrees Celsius (100.4F) or above with chills
- Cramping
Bleeding dark reddish or purple-colored rectal blood is also one of the diverticulitis symptoms. Bleeding is often mild and usually stops by itself; however, it can become severe. This usually occurs after intense diarrhea-like cramping pain, but fortunately, this is an uncommon diverticulitis symptom.
If diverticulitis is not treated properly, it can cause some serious complications, such as:
- Worsened abdominal pain
- No sign of fever dropping down
- Intolerance of any food or liquid. Any intake leads to vomiting
- Constipation for an extended period
- Distension of the abdomen
- Burning sensation while passing urine
- Rectal bleeding
Intense abdominal pain, particularly when it is limited to the lower left side or passing blood in the stool calls for medical attention. Seek medical care even if the bleeding stops on its own. It may not be diverticulitis however, it may be a sign of a serious disease.
Diverticulitis is not associated with weight loss. However, losing weight, passing rectal blood, and having frequent bowel movements, requires a visit to the doctor.
The diagnosis of diverticulitis
To confirm the nature of the disease, the medical practitioner would take note of the existing diverticulitis symptoms and will perform a physical exam. They may check for blood in your stool by doing digital rectal examination” in which a health-care professional inserts a gloved finger into the rectum to try to find a cause for bleeding or pain. A blood test might also be necessary to find out if the white blood cell count in the body is higher than normal.This is indicative of an infection. A CT scan using computer-guided X-ray images might be performed to check for infected diverticula.
Another test to detect diverticulitis is colonoscopy that is a procedure performed using a flexible tube with a tiny camera at the end, called an endoscope. The endoscope is inserted into the rectum and further up into the colon. It provides a direct view of the inner lining of the colon and rectum. The procedure is relatively painless and usually takes 30 to 45 minutes. Patients may be given a sedative medication to relax during the procedure. Sigmoidoscopy is another way to diagnose diverticulitis. It is performed with a flexible sigmoidoscope that has a tiny camera at the end of the sigmoidoscope. The patient lies on their left side while the instrument is inserted into the anus and advanced through the rectum and colon. This procedure is relatively painless and takes about 5 minutes.
Treatment for diverticulitis
The treatment is dependent on how bad the diverticulitis symptoms are. Doctors may prescribe treatment at home or if the condition is bad, then may suggest a hospital stay. Treatment at home would include bed rest and return to liquid diet first for the infection to heal. Gradually return to solid diet based on the doctor’s advice. Also, be very careful of taking the antibiotics and painkiller suggested by the doctor. Full recovery may take some weeks or some months based on the dietary and lifestyle changes after the treatment.

